Tackling mild depression: “iCBT was perfect for me.”
WHO
Telepsychiatry, also known as eMental health, is being used increasingly widely, especially in the form of internet-based cognitive behavioural therapy (iCBT). After an initial assessment to determine a patient’s suitability for iCBT, a doctor prescribes the online course, which is done segment by segment. The patient’s progress is monitored by a mental health professional who can be contacted at any time.
Providing iCBT for non-severe mental health difficulties such as mild depression and anxiety is becoming commonplace in Scandinavian countries as well as the Netherlands and the United Kingdom. Preliminary research indicates that, under the right conditions, it can be an effective alternative or complement to face-to-face therapy. It is inexpensive to provide and convenient for the patient, and can reach people living in remote locations who would otherwise have to travel very long distances to access therapy.
For Annika*, a teacher in her 60s living in the Helsinki area in Finland, it was the practicality of iCBT that attracted her when she began to notice signs that her mental health was suffering 2 years ago.
Access to therapy 24/7
“I started to be very upset and everything seemed to be too much. I managed at work with no problems, but at home I got hurt very easily and would start crying or screaming at my husband, no matter what he said. I felt so tired I started to hide from situations and I wasn’t going to see our children and grandchildren because of it. I tried to see a psychologist but I found the appointment times very difficult. I was busy, she was busy. She seemed to think that because I was busy I must be OK, but I wasn’t.”
Annika wanted to be able to access therapy at the times that suited her, including in the middle of the night if she couldn’t sleep, so her doctor referred her to MentalHub.fi.
“From the very first day I noticed how manageable it all seemed. I made my activity diary and it helped me understand that thoughts affect emotions. My automatic thoughts were negative and critical, so I needed to change my internal dialogue. I realized I was demanding more and more of myself because I wanted everything to be perfect. Of course everything can’t be perfect all the time and I have learned to say no and to delegate. You have to be your own best friend and start treating yourself that way.”
It took Annika 7 months to get through the course, during which time her progress was monitored.
“Your own therapist reads everything and she sees if you have done your exercises. I don’t have a problem with being open but privacy is important and it’s actually helpful that it’s only one person that you don’t actually know. I didn’t write to her often but she always answered quickly. When you’re feeling overwhelmed, it’s actually a relief that you don’t have to talk to anyone.”
Taking action to improve her mental health before things became any worse turned out to be especially important, because a tragic event was just around the corner for Annika.
“When my mental state is good, I am good at recovering, physically and mentally. My godson died of heart failure on the 1st of November, the day before he turned 40. He was like my own child. It upset me enormously and if it had happened while I was feeling depressed I think it would have killed me. But I’ve been able to manage and it’s all thanks to the therapy. I have been able to help the rest of the family and concentrate on all the good wonderful things we had together. My godson and I had a very serious talk in October and we told each other how we loved each other. If I had been depressed perhaps we would never have had that talk. Despite the bereavement my anxiety and depression levels are zero; iCBT was perfect for me.”
Telepsychiatry can relieve pressure on mental health services
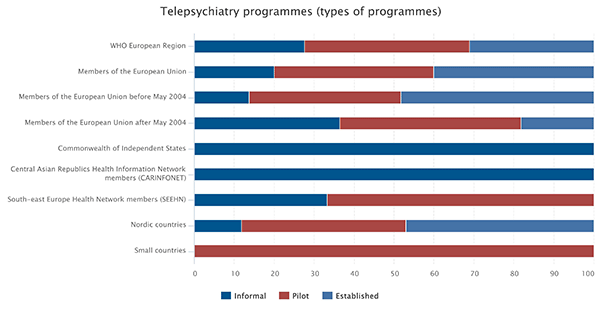
The results of the 2016 report “From innovation to implementation: eHealth in the WHO European Region” show health systems across Europe making great progress towards establishing telepsychiatry programmes, especially in Nordic countries and the countries that were members of the European Union prior to 2004. Pilot programmes are also becoming commonplace in south-eastern Europe, in the small countries (those with a population of less than 1 million) and among the newer members of the European Union.
Clayton Hamilton, Leader of the eHealth and Innovation Unit of the Division of Information, Evidence Research and Innovation at WHO/Europe, points out: “In terms of the burden of disease, the impact of depression on individuals and on society as a whole is significant and becoming increasingly so. Telepsychiatry can extend the possibility of therapy to a large number of people at a fraction of the cost of face-to-face therapy. Of course it’s not suitable in every case and needs to be carefully prescribed by a mental health professional but, when properly applied, it can make a huge difference, extending the reach of mental health services and relieving pressure on overburdened health systems.”
* For the purposes of this interview, a pseudonym has been used.