Moving towards a multisectoral approach to tackling antimicrobial resistance
A new publication produced by WHO’s European Observatory on Health Systems and Policies and published by Cambridge University Press outlines the need for multisectoral approaches – involving disciplines such as human medicine, veterinary medicine, agricultural sciences, epidemiology, economics, sociology and psychology – to address the global problem of antimicrobial resistance (AMR). The publication goes on to describe the potential economic and policy responses for tackling the challenge of AMR in the European Union.
It is widely acknowledged that antibiotics revolutionized medicine. Over time, however, available antibiotics and related drugs are becoming less effective and pathogens are becoming more resistant. WHO has identified AMR as one of the top global health challenges facing the world today.
The book is part of a new series focusing on critical issues in the transformation of health systems in Europe – a process being driven by changing environments, increasing pressures, and evolving patient and societal needs. Each study aims to provide both practical and policy-relevant information and lessons on how to implement change to make health systems more equitable, effective and efficient.
Antimicrobial resistance
The health burden of infections caused by AMR in the European Union is similar to that of influenza, tuberculosis and HIV/AIDS combined. In 2015, there were 670 000 antibiotic-resistant infections in the European Union, which resulted in 33 000 deaths.
The problem reaches far beyond the EU. The misuse and overuse of antibiotics worldwide are accelerating AMR. Between 2000 and 2015, global antibiotic consumption for human health increased by 65%.
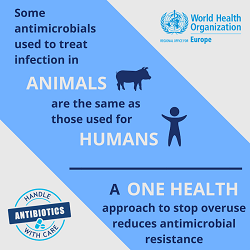
Over 70% of antibiotics consumed worldwide are given to livestock. Between 2000 and 2018, the proportion of antimicrobials showing resistance levels greater than 50% more than doubled in chickens and pigs globally.
Multisectoral action to tackle AMR by addressing the interconnection of human, animal and environmental health is known as the One Health approach.
Economic and policy responses for One Health
The research underpinning policy options to tackle AMR is rapidly evolving across multiple disciplines such as human medicine, veterinary medicine, agricultural sciences, epidemiology, economics, sociology and psychology.
Skewed economic incentives have slowed the development of novel antimicrobials and limited efforts to reduce antimicrobial usage. This points strongly to the need for greater innovation and investment for research and development of new antimicrobial medicines.
Tackling AMR in the community, where 90% of antibiotics for human use are prescribed, involves working at different levels of the system to support change. Examples include reducing the amount of antibiotics prescribed by doctors and changing patient expectations regarding antibiotics. Addressing AMR in hospitals relies on robust infection control measures as well as education, regulation and transparency.
Many countries, such as Belgium and the Netherlands, have achieved a dramatic reduction in antimicrobial use in animals. Reducing AMR in the food and livestock sector is possible by:
- preventing the use of unnecessary antibiotics;
- ensuring greater biosecurity;
- improving husbandry methods;
- using vaccination; and
- reserving critically important antimicrobials for human use only (currently, most antimicrobials are used for both humans and animals).
Improved use of diagnostics holds significant potential to tackle AMR, as does vaccination. Vaccination works directly by preventing infection, but it also works indirectly – vaccinating against one pathogen may reduce the risk of infection with another interacting pathogen.
The positive news is that a wide range of multisectoral policy options are available to policy-makers. This volume brings together the latest evidence on the different ways to tackle the complex problem of AMR.



