Women and cancer: screening and treatment save lives

WHO/Kanti Kumar
One in five women in the WHO European Region will get cancer before the age of 75. In terms of the share of total incidence, the eight most important types of cancer among women in the Region are:
- breast (28.0%)
- colorectal (13.2%)
- lung (6.7%)
- uterine (5.8%)
- ovary (4.3%)
- stomach (4.1%)
- cervical (3.8%)
- pancreatic (3.0%).
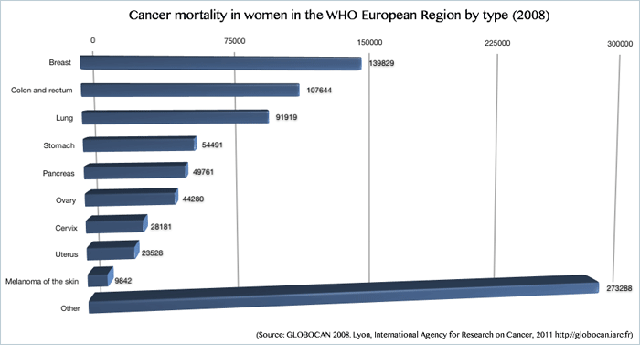
Cancer mortality presents a slightly different picture, however. In terms of the share of total cancer deaths, the most important types are:
- breast (17.0%)
- colorectal (13.1%)
- lung (11.2%)
- stomach (6.6%)
- pancreatic (6.0%).
WHO supports countries in implementing the four basic components of cancer control – prevention, early detection, diagnosis and treatment, and palliative care – to prevent and cure many cancers, and alleviate suffering.
Enough is already known about the causes to prevent at least one third of all cancers. Key measures include implementing tobacco-control measures, maintaining a healthy body weight and conducting population-based screening (for example, for cervical cancer).
Some of the most common types of cancer among women – including breast, colorectal and cervical cancer – can be cured if detected early by the health system. The early detection of these three is one of the priority interventions of the Action Plan for Implementation of the European Strategy for the Prevention and Control of Noncommunicable Diseases 2012–2016, endorsed by the 53 countries in the WHO European Region in September 2011.
Early detection requires population-based screening programmes and greater awareness of the early signs and symptoms of cancer. Prompt follow-up through referral and treatment is essential.
“We must move away from the idea that women’s health simply means maternal health, for and during pregnancy. Cervical cancer is preventable; other cancers are treatable if detected early, and it is our duty to do everything we can to ensure that lives are saved,” said Dr Gunta Lazdane, Programme Manager, Sexual and Reproductive Health, WHO/Europe.
Cervical cancer: vaccination and screening
WHO calls on countries to introduce organized, population-based screening for cervical cancer, which could prevent 80% of cases. (Screening reveals pre-cancerous changes in the cervix.)
In addition, an effective vaccine exists to protect women against human papillomavirus (HPV), the primary cause of cervical cancer. Many countries in the WHO European Region have introduced or are introducing HPV vaccine into their vaccination programmes.
Over 100 experts and policy-makers from 42 countries and 7 partner organizations gathered in Istanbul, Turkey in October to discuss the prevention of cervical cancer in the WHO European Region. The experts agreed that both vaccination and screening are important: one does not preclude the other, and health systems should offer both.
Challenges remain, however:
- ensuring women’s understanding of the importance of screening, and equal access to screening services; and
- covering the cost of the vaccine and overcoming cultural sensitivity about it.
Clear communication about the benefits of the vaccine is vital for broad uptake, and several countries have run successful campaigns combining cervical screening for mothers, vaccination for daughters and strong communication activities.
The introduction of the HPV vaccine as part of the Netherlands’ immunization programme in 2009 faced strong resistance from many quarters, including scientists who argued it was too early to use the vaccine. The Ministry of Health, Welfare and Sport changed its communication strategy about the vaccine to counter rumours and opposition.
“What we learned from the first phase of the introduction of HPV vaccine is that we should promote a dialogue with target groups, and address uncertainties and emotions,” said Dr Marina Conyn of the National Institute for Public Health and Environment (RIVM) in the Netherlands. “We have to emphasize that this is different from polio vaccination, where we want high vaccine coverage to ensure group immunity, and prevent outbreaks from occurring. Here it is about individual protection, and people have to decide now to prevent something in the future. We try to explain that, if you aren’t vaccinated, you can of course still be in the screening programme. We really emphasize, though, that both vaccination and screening are important in preventing cervical cancer.”
Breast cancer: early detection and treatment
As mentioned, breast cancer is the most common type among women in the European Region, but its share of cancer mortality is lower, due to improvements in screening and developments in treatment.
From 1950 to the late 1980s, breast cancer mortality continually rose throughout the European Region, with a few exceptions (Norway, Sweden). This trend was reversed in the 1990s, with rates decreasing or at least levelling off in most countries by 2004.
On 15 October 2011, WHO brought together experts in Turkey to discuss advances in breast-cancer detection and treatment, and the challenges in ensuring screening and timely treatment. The experts highlighted the increased incidence of breast cancer in developing countries, where 60% of deaths now occur. Projections indicate that the breast-cancer burden in Turkey and developing countries will continue to rise.
Recognizing the early signs and symptoms is vital for diagnosis and early treatment. A range of techniques (breast self-awareness, clinical examination and mammography) are in use for early detection. Once cancer is detected, the health system must have the capacity for appropriate treatment.
Nevertheless, fear remains a big barrier to regular screening. Professor Riccardo Masetti, Director of the Interdepartmental Centre for Breast Diseases at the University of Rome, Italy, used his country as an example: more than 55% of women did not turn up for screening, despite being informed of its importance. “It is difficult to remove the fear; it is easier to avoid creating it by working with and educating young people, allowing them to understand the importance of taking care of their health,” he said.
Among the other barriers identified is the lack of access to screening facilities and medical professionals. In Turkey, for example, there are fewer than 200 oncologists for the population of 72 million people. The national cancer programme now aims to build 54 multidisciplinary cancer centres in the country by 2020.
With the Turkish Ministry of Health, WHO used the 33rd Intercontinental Istanbul Eurasia Marathon, on 16 October 2011, to raise awareness about breast-cancer screening and treatment. People were invited to participate in “Walking for the cure” as part of the Marathon, in which thousands of people walked and ran.