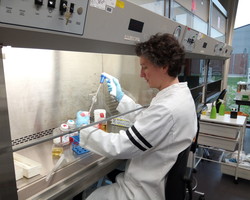
Dr Jelke Fros, virologist, the Netherlands
Jelke Fros
Jelke Fros
Currently available vaccines protect children and adults against over 20 life-threatening diseases, and vaccines in the pipeline have the potential to expand this protection to even more diseases, including HIV and norovirus. At the same time, fundamental research continues to pursue knowledge that could lead to new generations of vaccines, potentially for diseases that are not yet known.
Dr Jelke Fros is among researchers at Wageningen University in the Netherlands and elsewhere who are aiming to better understand how viruses and hosts (like us) try to outsmart each other. This work has the potential to fundamentally change how, and how quickly, vaccines can be developed in response to new public health threats.
Dr Fros explains: “Cells and viruses are intertwined in a constant battle. When a virus enters a cell, the cell tries to recognize and eliminate the virus; while the virus has adapted to hide, evade and block the cellular responses. We are looking at how this interplay between virus and host has evolved and how we can use this to our advantage”.
Aiming at a moving target
Development of a new vaccine normally requires decades of research and testing. Responding to viruses that emerge in a new place without warning, like Zika, or that mutate quickly, like influenza, therefore poses special challenges. “With changing environments, we see multiple examples of viruses that either show up out of nowhere or move to a place where they have not been seen before. The need for rapid development of novel vaccines has increased.”
The long-term aim of Dr Fros and his colleagues’ research is therefore to develop a platform through which vaccines can be developed rapidly against a multitude of viruses, based on understanding how the viruses’ genetic code has evolved and how the host responds to them.
“Zika is one of the models, but we are currently looking at the genome evolution of viruses in general and how this has been shaped by the host’s immune responses. We are trying to alter the genome of viruses in such a way that host cells better recognize these viruses, which will stimulate immune responses,” says Dr Fros.
This new approach could theoretically be applied to many different viruses, drastically reducing the time that passes between the emergence of a new pathogen and the development of a safe and effective vaccine to protect against it. With personal experience testing samples for Ebola in Sierra Leone during the outbreak in 2015, Dr Fros is well aware of the potential to save many lives.
One step at a time
“This field of research is still in its infancy,” cautions Dr Fros. Recent discoveries by a number of research groups have resulted in a better understanding of an immune pathway that can recognize virus genomes in a certain way. “With multiple groups now studying this pathway, hopefully that can lead to some kind of vaccine platform in the future. The main point is to first understand the innate immune responses that are involved and to determine whether results obtained for one virus also apply for other viruses.”
“Ideally we would have a platform ready that only requires easily obtained information about newly emerging viruses, apply a single approach to make specific changes to these viruses and directly test these vaccine candidates. We are not there yet, but I really think there are possibilities to create such a technology that is applicable for many viruses, which is why we are looking into this.”
In the meantime…
What does fundamental research look like? “Mostly it’s lab work. Together with a group of people, we go into the lab and investigate interactions between host immune responses and viruses. We use different cell lines and infect them with viruses. We often make specific changes to the viruses or the cells to see what effect these changes have on virus replication and the cells’ immune responses. For some of the models, such as Zika virus, we use a specialized BSL [biosafety level] 3 laboratory. In this laboratory, we also investigate how these viruses are transmitted by mosquitoes, which requires us to wear specific personal protection, so we are completely covered in plastic.”
Fundamental research involves long-term thinking about what may be possible in the future. These days, Dr Fros is also thinking a lot about the vaccines available today. “Good vaccines are important to protect people, including newborns. My daughter is just 5 days old and I’m depending on everyone around her to be vaccinated so she’ll also be protected until she can be fully vaccinated herself.”



